Our MSK Outpatient Service provides physiotherapy for patients presenting with physical conditions caused by accidents, illnesses and the ageing process. We also provide treatment for patients with pelvic health and chronic pain conditions.
We offer a flexible model of service delivery with both virtual (telephone or video) and face-to-face (F2F) appointments based on your clinical need and/or personal choice. When planning your care, we want to know what matters most to you. Your physiotherapist will carry out an assessment and examination of your problem and then work with you to determine your treatment goals and how we can best support you to achieve them.
Depending on your condition, Physiotherapy can involve a range of different treatment options to assist you in restoring movement and strength, manage pain and improve function.
You will usually be seen by the same Physiotherapist each time you attend. We are a teaching hospital and students work under close supervision of a Senior Physiotherapist. If you do not wish to be seen by a student, please let us know.
If it is your first appointment, your physiotherapist will carry out a 30-40 minute assessment to determine the nature of your problems and work with you to develop a treatment plan.
You will be asked questions about your current condition. These may include:
- The history of your condition and any activities that affect your pain
- Medication
- Medical History
- Your occupation, hobbies or interests and how they are affected
You may also be asked general questions about your physical and mental health and wellbeing e.g. in relation to your weight and how physically active you are.
Please wear loose and comfortable clothing and be aware that you may be asked to undress so the physiotherapist can examine the affected area. For example, if you have a leg or back problem, please bring shorts to change into.
Following your initial assessment your physiotherapist will discuss a treatment plan with you. This will usually include an exercise programme for you to follow at home and information/ advice on how to access physical activity and exercise sessions within your local community.
Any follow up appointments will last around 20 minutes and be more targeted on following the plan set from the first appointment.
If a telephone or video appointment has been arranged, a physiotherapist will call you. During the call, we will be able to discuss your condition and give appropriate advice. You may be given another virtual appointment or be asked to attend a face-to-face appointment in the clinic. For virtual appointments please make sure you are in a quiet area where you will not be disturbed. You will also need space to move around same as you would for a face to face appointment.
MSK Physiotherapy Admin Office
For any enquires, or if you need to make or cancel an appointment, please phone the MSK Physiotherapy Admin Office on:
Phone line: 0161 778 3882 1. (Lines are open Monday to Friday 07:30-16:00)
Our core hours are Mon - Thurs, 7.30am - 6pm; Fri 7.30am - 4pm
Or email us at: FGHphysio@nca.nhs.uk
If you cannot attend your appointment, please give 24 hours' notice by either contact method. Due to high demand on our services, if you fail to attend your appointment and have not contacted us you may be discharged in line with the Trust access policy.
Patient feedback: Your feedback is important to us, as we are constantly aiming to improve our services. Please click ‘Patient feedback form’ or scan the QR code below.

Physiotherapy Department, Fairfield General Hospital, Rochdale Old Road, Bury, BL9 7TD.
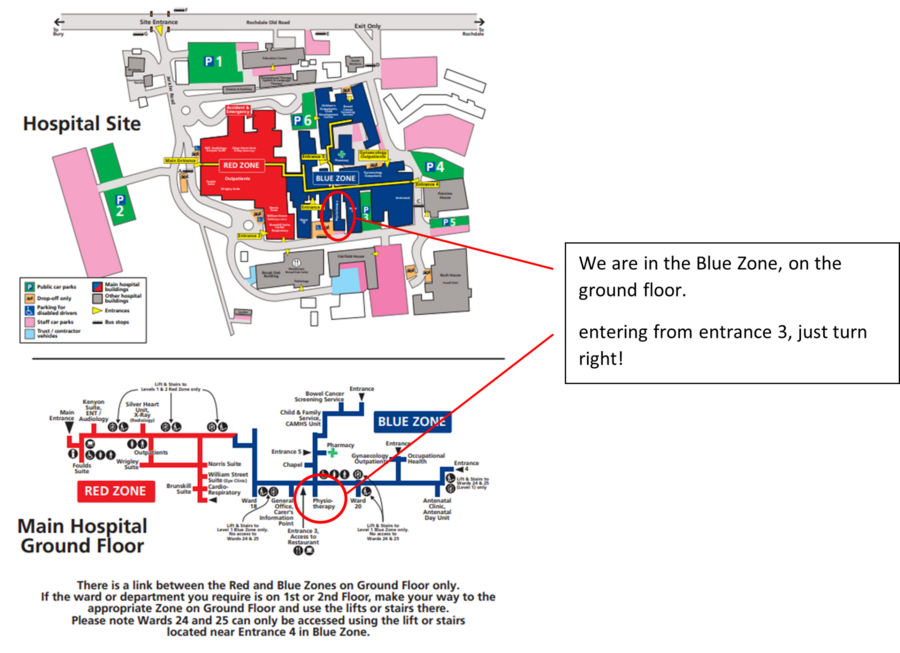
If you are planning to arrive by car, please allow yourself adequate time to park as it is sometimes difficult to find suitable parking during the day. Please be aware that the hospital operates a ‘Pay & Display’ system for parking. The nearest disabled parking is at entrance 3.
The nearest entrance for the Physiotherapy department at Fairfield General Hospital is entrance 3 however please be aware that there is only disabled parking outside this entrance.
Your Feedback Matters! At Fairfield General Hospital, we value your experience. Your feedback helps us enhance our services and care. Share your thoughts with us to help us continue providing exceptional healthcare tailored to your needs. Your input shapes our commitment to excellence. Thank you for being part of our journey to better healthcare.
Please click to fill out our feedback survey or scan the QR code!

- Bury Exercise and Therapy Scheme/Bury Livewell Services : https://www.bury.gov.uk/livewell
- Bury Directory: https://www.bury.gov.uk
- Healthy Minds: https://www.penninecare.nhs.uk/healthymindsbury
Further Guidance
Neck pain is extremely common. In their lifetime, 40–70% of persons will experience a substantial episode of neck pain. While there may be a history of injuries, such as from a vehicle accident, it frequently develops for no apparent reason. Persistent neck pain is linked to being overweight, adopting bad posture and mobility during the workday, and experiencing high levels of stress.
Sometimes tingling, numbness, and arm discomfort can coexist with neck pain. This could indicate that a nerve in the neck is irritated. Even in these cases, discomfort normally goes away on its own over a few weeks or months, requiring no special treatment. Should you experience a recent onset of weakness in your arms or legs in addition to neck pain, you should speak with your general practitioner.
Shoulder pain is a common problem in adult life. It can be the result of an injury or it can start without a known cause. Often shoulder pain responds well to simple advice and self- management. The shoulder joint is the most mobile joint in the body. It’s a ball and socket joint which enables a very wide range of movement supported by the rotator cuff muscles and tendons.
Common diagnosis we treat are:
Subacromial Pain
Subacromial pain syndrome is an umbrella term for pain that starts in the shoulder and can travel down the arm or to the neck. It is the most typical cause of shoulder discomfort. It could develop due to injury, trauma, repetitive strain, age related changes or sometimes, without any reason. The main symptom is pain in the upper arm caused by specific movements or activities. These are usually activities that involve lifting the arm above shoulder level and reaching behind the back, for example when putting a jacket on.
Frozen shoulder
Frozen shoulder, also known as adhesive capsulitis, is a painful condition that results in stiffness of the shoulder joint. A frozen shoulder can develop without any cause but it can also occur after an injury or surgery. The shoulder joint is surrounded by a joint capsule. The joint capsule is normally flexible and loose which allows the shoulder joint to move freely. In a frozen shoulder the capsule becomes thickened and inflamed. This causes the shoulder to become painful and stiff. Frozen shoulders can get better in time without any treatment. There are treatments that can help with the pain and to maintain or improve your shoulder movement. These include pain relief and gentle exercises.
Degenerative Rotatorcuff tear
The rotator cuff muscles interlock to work as a unit. They help to stabilise the shoulder joint and help with shoulder joint movement. The four tendons of the rotator cuff muscles join to form one larger tendon, called the rotator cuff tendon. This tendon attaches to the bony surface at the top of the upper arm bone (the head of the humerus). As we age the rotator cuff can be susceptible to degenerative changes which could then cause a defect in the tendons. The onset is usually gradual over many years and often unnoticed as the shoulder compensates for it. 20-40% of people in their 60’s function normally with this with no pain or noticeable weakness.
Trauma, repetitive movements, overuse injuries can often result in elbow pain, however pain could also start gradually without a known cause. The elbow joint is a hinge joint that connects the forearm's radius and ulna to the upper arm's humerus. Elbow pain problems often respond well to simple advice and self- management.
Common elbow pain diagnosis include:
Tennis elbow (lateral epicondylitis)
Usually on the outer elbow where the forearm muscle tendons attach on or around the lateral epicondyle. It is typically made worse when making a strong grip or with wrist movements. Pain can radiate down the forearm and occasionally above the elbow into the upper arm. Evidence has shown that exercise can be very effective at reducing pain and improving use of the arm.
Golfers elbow (medical epicondylitis)
Usually on the inner elbow where the forearm muscle tendons attach on or around the medial epicondyle. It is typically made worse when making a strong grip or with wrist movements. Pain can radiate down the forearm and occasionally above the elbow into the upper arm. Evidence has shown that exercise can be very effective at reducing pain and improving use of the arm.
The hand needs a complex network of tendons to function as a unit in order to move. These tendons are located next to several nerves that provide us hand sensation, strength, and touch. The wrist and hand complex may move and function abnormally if any of these structures are damaged, and pain may arise during specific activities.
Common hand diagnosis include:
DeQuervains
De Quervain’s disease causes pain when you move your wrist and thumb, and usually a tender swelling at the base of your thumb. Two of the tendons that move your thumb usually glide freely through a tight tunnel at the base of your thumb. If the tunnel thickens and becomes too tight, it becomes painful to move your thumb and you may experience stiffness or locking when you move it.
Carpal Tunnel
The carpal tunnel is a channel at the wrist that runs between the bones and a strong band of connective tissue. Within this tunnel, you have blood vessels, the median nerve and several tendons that help you move your fingers and wrist. When the median nerve runs through this tunnel, it can be compressed and may result in carpal tunnel syndrome. Symptoms of carpal tunnel syndrome include pain, a tingling sensation, numbness and/or a burning sensation in the hand or fingers. Usually worse at night or first thing in the morning, gripping objects or continuous use of the hand like typing.
Base of Thumb Arthritis
Thumb arthritis is osteoarthritis, which is loss of the smooth cartilage surface covering the ends of the bones in the joints. The cartilage becomes thin and rough, and the bone ends can rub together. Osteoarthritis can develop at any age, but usually appears after the age of 45. Intense pain, swelling, and a reduction in strength and range of motion can result from thumb arthritis, making it challenging to do daily activities like opening jars and turning doorknobs.
The lower back (lumbar spine), is made up of 5 spinal bones called vertebrae. These bones are then surrounded by strong muscles and ligaments to allow it to move and to protect it from harm. Inbetween the vertebrae we have lumbar discs, which are fully attached to the bone and ligaments. The discs never ‘slip out of place’, although this term is a popular way of describing both back pain and sciatica.
In the vast majority of cases, as many as 95%, it will not be possible to find a specific cause for back pain. This means no single joint, ligament or muscle is causing the pain. For this reason, most low back pain is referred to as ‘non-specific’. Spinal experts around the world have agreed on this term. It means that we think that the spine isn’t working well as a whole and that safely practiced movement will help it get back into its natural pattern. Non-specific low back pain can sometimes last a long time, called chronic low back pain.
Back pain is a very common condition that can strike people of any age. Most people get better on their own and don't really need any additional care. For some people, movement, exercise, and physiotherapy can significantly aid in pain relief and can return to regular activities. Surgery and imaging are rarely thought to be beneficial for back pain. There has been a lot of research in recent years which has changed the thinking about the best way to deal with back pain.
Sciatica
Sciatica results of inflammation of the sciatic nerve in the lower back which goes down all the way into the foot. It has become an umbrella term now for a majority of nerve related pain in the lower back. A medical term we can use to describe this is lumbar radiculopathy. Nerve irritation can cause leg pain (at times very severe), sensitivity, pins and needles, numbness, weakness or a combination of symptoms. For most people the pain reduces in around 12 weeks. Some people find the symptoms settle of their own accord, some may need help from their GP or a physiotherapist. Exercises and medications, prescribed by a health professional, can help to ease pain and improve mobility as your sciatica heals.
Stenosis
Lumbar stenosis is caused by normal age related ages in the spine. We may get enlargement of the joints, ligaments and discs can bulge as well. As scary as this sounds, this is a normal finding. However, in some people it narrows the space for the nerves that pass down the low back and into the legs – causing symptoms like pain, weakness and tingling that we feel in the legs. Unlike sciatica, the leg symptoms are often only present when using the legs, such as walking and standing, and ease quite quickly when you rest.
The hip joint is one of the largest weight-bearing joints in the human body and plays a crucial role in various movements, including walking, running, and jumping. It's a ball-and-socket joint formed by the head of the femur (thigh bone) and the acetabulum of the pelvis. The ball-shaped head of the femur fits snugly into the socket of the acetabulum, allowing for a wide range of motion. Strong ligaments and muscles surround the hip joint, providing stability and support. The hip joint is also lined with cartilage, which helps cushion the bones and facilitates smooth movement. Overall, the hip joint is essential for mobility and bears significant loads during daily activities.
Hip osteoarthritis
Another way to think of arthritis is as typical wear and deterioration. This could have been found with an x-ray or after a hip evaluation. It's not always the case that osteoarthritis will worsen after a diagnosis. Osteoarthritis is a normal part of ageing, just like wrinkles or grey hair. The second most frequent joint to develop arthritis in is the hip. In younger people, secondary arthritis may develop if there has been prior trauma or dysplasia (a congenital malformation of the joint).
Lateral hip pain
Also known as Greater Trochanteric Pain Syndrome is an umbrella term for trochanteric bursitis, external coxa saltans (ie, snapping hip), and abductor tendinopathy. Patients with greater trochanteric pain syndrome (GTPS) usually complain of pain at the side of the hip radiating down the side of the thigh and sometimes below the knee.
- It is more common in females
- More common in 40-60 year old patients
- Occurs in 10-25% of the population
- Occurs in 35% of patients with low back pain
Adductor tendinopathy
Tendinopathy indicates a problem with the tendon, which can involve degeneration, inflammation, or injury. Symptoms of adductor tendinopathy may include pain in the groin or inner thigh area, particularly with activities that involve using the adductor muscles, such as running, kicking, or jumping. There may also be stiffness, swelling, and tenderness in the affected area. Treatment for adductor tendinopathy typically involves a combination of rest, ice, physical therapy, stretching and strengthening exercises, and modifications to activity levels to allow the tendon to heal.
The knee joint is one of the largest and most complex joints in the human body, providing essential support and flexibility for activities such as walking, running, and jumping. It's a hinge joint formed by the articulation of three bones: the femur (thigh bone), the tibia (shin bone), and the patella (kneecap). The ends of these bones are covered in smooth cartilage, which helps cushion the joint and facilitate smooth movement.
Anterior knee pain
Anterior knee pain refers to discomfort or pain experienced at the front of the knee, typically around or behind the kneecap (patella). It's a common complaint and can occur due to various reasons, including overuse, muscle weakness, poor biomechanics, or underlying medical conditions such as patellofemoral pain syndrome or patellar tendinitis. Symptoms of anterior knee pain may include a dull ache, sharp pain, or a feeling of pressure around the front of the knee, especially during activities like running, climbing stairs, or sitting for prolonged periods with the knees bent. Swelling, stiffness, and a sensation of grinding or clicking in the knee may also accompany the pain.
Patella tendinitis
Patellar tendinitis is an overuse injury affecting your knee. It is the result of repeated overstress of your patella tendon beyond its coping capacity. A common name for it is Jumper’s Knee since it is common in sports involving jumping. Usually start with pain and inflammation of the tendon. Commonly it does not heal as nicely as we would like it too and is still painful on exertion, at this point it may be referred to as patella tendinopathy.
Meniscus
The meniscus is a C-shaped piece of cartilage that acts as a cushion and stabilizer within the knee joint. It sits between the femur (thigh bone) and the tibia (shin bone), helping to distribute weight and absorb shock during movement. The meniscus also aids in lubricating the joint and providing stability, allowing for smooth and pain-free motion. However, it can be susceptible to injury, particularly through twisting or sudden movements, leading to pain, swelling, and restricted movement in the knee. This is known as an acute meniscus injury or tear. Another way the meniscus could present with pain is with age related changes, known as a degenerative meniscus tear. Physiotherapy would generally aim to strengthen up all the supporting structures as much as possible, with is to reduce symptoms.
The ankle and foot form the foundation of our body's movement and support. The ankle joint is where the lower leg bones (the tibia and fibula) meet the talus bone of the foot, enabling actions like walking, running, and jumping. Ligaments surrounding the ankle provide stability and support.
The foot consists of multiple bones, muscles, ligaments, and tendons that work together to facilitate various movements and activities. Muscles and tendons in the foot and ankle coordinate to support the body's weight, provide propulsion, and maintain balance on various surfaces.
Ankle sprain
When we sprain or roll over the ankle, the ligaments most likely to be injured are the lateral ligament complex which are situated on the outside aspect of the ankle, running from the ankle bone and fanning downwards to attach onto the foot. Like all ligaments, it’s purpose is to act like a seatbelt, preventing excess movement at the joint. The lateral ligament complex of the ankle is the most commonly injured set of ligaments in the body.
Fortunately, this group of ligaments heals quite well and usually always recovers totally without the need for surgery or other treatments. Both its blood flow and nerve supply are excellent, which contribute to its rapid healing.
You may also experience significant bruising which may appear in the same place as the pain but may also be some distance from the injury – either near the bottom of the foot or higher up the calf. This is normal and more related to the position that it has been kept in.
Achilles tendinopathy
Achilles tendinopathy refers to a condition involving pain, stiffness, and sometimes swelling in the Achilles tendon, which is the large tendon located at the back of the ankle, connecting the calf muscles to the heel bone.
This condition typically occurs due to overuse or repetitive strain on the Achilles tendon, commonly seen in athletes who engage in activities involving running, jumping, or sudden changes in direction. It can also result from improper footwear, inadequate warm-up or stretching, or biomechanical issues such as flat feet or tight calf muscles.
Symptoms of Achilles tendinopathy may include pain and stiffness in the back of the ankle, especially during physical activity or after prolonged periods of rest. The area around the tendon may also feel tender to the touch, and in severe cases, there may be swelling or thickening of the tendon.
Treatment often involves rest, ice, and anti-inflammatory medications to reduce pain and inflammation. Physical therapy exercises may be prescribed to strengthen the muscles surrounding the tendon and improve flexibility. In some cases, orthotics or changes in footwear may be recommended to alleviate pressure on the Achilles tendon.
Plantar fasciitis
Plantar fasciitis is a common foot condition characterized by inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of the foot, connecting the heel bone to the toes. Symptoms of plantar fasciitis include stabbing pain near the heel or along the arch of the foot, particularly during the first steps in the morning or after prolonged periods of standing or walking. The pain may improve with activity but worsen again after rest.